My training for the Sydney marathon really kicked off when I landed back home in May, after running up and down mountains in Latin America for 8 months.
I was hoping the “altitude training” would pay off with only 4 months until the one marathon where I had the chance to qualify for the Boston Marathon in April 2017.
For Boston I had to run at least 3:35 in Sydney, with no guarantee that time would be fast enough to get me there. The faster you ran above the qualifying time, the higher your chance of getting accepted.
Getting into the Boston Marathon is like getting the golden ticket in a Willy Wonka chocolate – a runner’s dream.
I wasn’t as disciplined as I was for the NY marathon, in the sense I didn’t follow a specific marathon training plan but decided to do a self-made routine of long runs, sporadic sprint training, strength training, high intensity interval training and some much needed yoga. My approach was, run a lot, get a little bit stronger and a little bit faster.
I had a few races in between Sydney – the Nike Women’s Half marathon, the Sydney Harbour 10K, the Sydney City2Surf 14K and a final 35K trail race 2 weeks out from the marathon – I PR’d in all of these but the races push you to your limits and can tire you out. So that was more than enough for me.
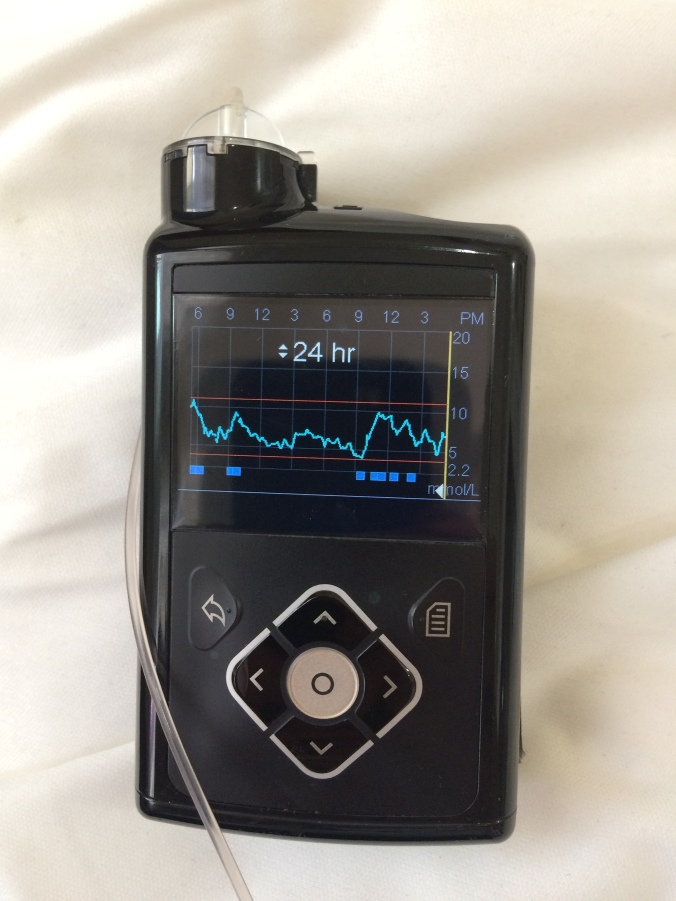
My BGLs were relatively well behaved until I started my new job a month after returning home, and switched my routine from morning runs to post-work evening runs. I started having high BGLs in the morning after breakfast that would continue throughout the day.
I was trying to get my BGLs in check and refuel from my intense training schedule at the same time. Let’s just say, my fuelling strategy was not up to scratch. I was restricting my usual carbohydrate intake. Only when I returned to my morning run routine did my BGLs improve dramatically and increase my insulin sensitivity.
Leading up to race day I was feeling good, not as strong as I would have liked to be and a little tired (mostly mentally), but I had my eye on the goal and felt my training had me in a good position for a good result.
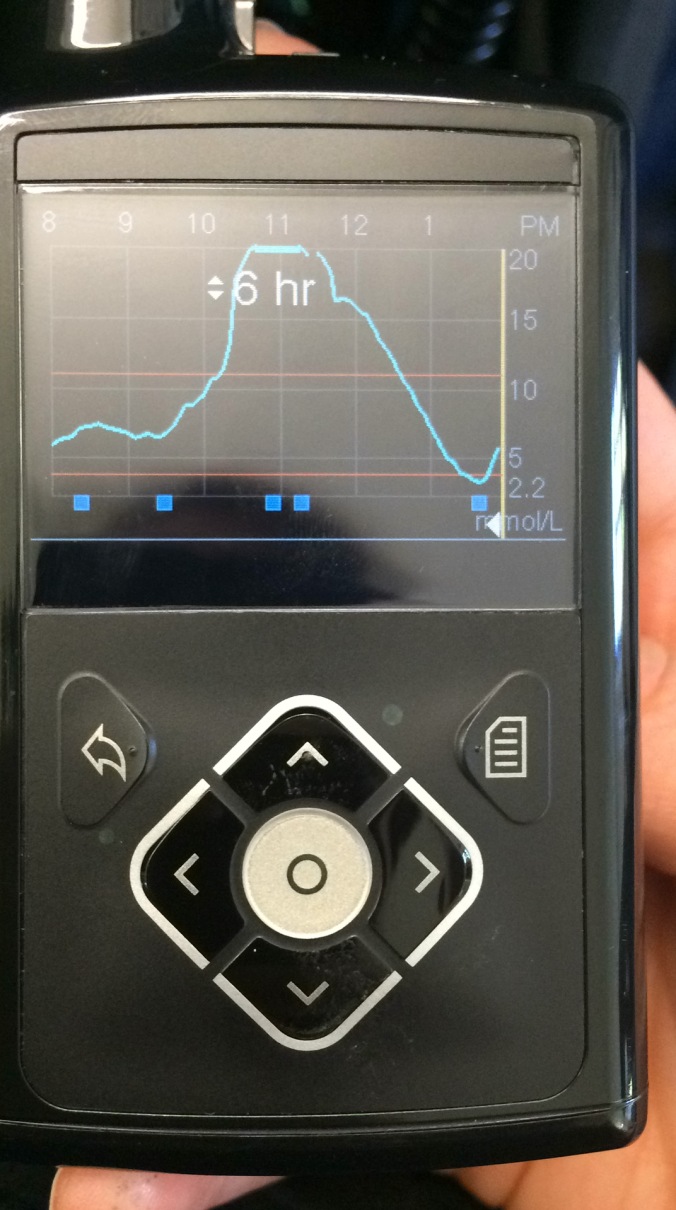
Race day started at 3am when I woke up after a very restless sleep with a BGL of 9mmol/L and ate a bowl of buckwheat groats, almond milk and some strawberries. Back to bed for 2 hours and back up at 5am with a BGL of 5mmol/L, dressed and a banana in hand I headed out the door.

I was lucky enough to be in the front group of runners just behind the elites, so crossed the start line just after 7am with a BGL of 13mmol/L. I always want to start a race with a BGL of approx. 200. No pre-race snack was needed, but I had plenty in my waste belt, just in case.
I started out fast and feeling good. Weaving in and out of fellow runners and setting a good pace of approx. 7:25 per mile. I managed to keep this pace up until mile 20, even after stepping on a stone and bruising the bottom of my foot at the half way mark.
At mile 5, I gave 0.3 units of insulin to get my BGLs down a bit so I could refuel with a Clif bar and some apricot bites 30 minutes later. I kept my BGL between 8-10mmol/L most of the race. Not wanting to risk letting it go too low.
Just before mile 20 as I was coming up a small hill, I saw my Dad cheering me on “GO AMES, you can run a 3:20”.

This gave me just the energy boost I needed as my legs started to tire and my mind struggled to filter out the pain.
It was great having the support of my Dad, who got up early just to get to the side line in enough time to cheer me on.
The last 7 miles were tough. My BGLs were okay, so I didn’t plan on eating any more food unless they started to drop, even though I had only consumed approx. 70g of carbs the whole marathon. Recommended fuelling is 20g of carbs every 20mins.
I was getting thirstier at each water station and drinking more to try and stay hydrated enough to take me to the finish line.
I hadn’t hit the wall but my legs definitely didn’t want to move any faster and the ball of my foot was hurting from that damn stone.
I knew if I could keep my pace I would be closer to a 3:20 finish.
For the last 5 miles I focused on getting to the next mile, perhaps repeating “Boston” in my head over and over. I tried to stay in a positive mindset and push through the pain.
The last mile I used all the adrenaline in my body to speed up and cross the finish line in 3:25:56 – 14 minutes faster than NY and 9 minutes faster than the official Boston qualifying time.

And most importantly my BGL was nicely sitting at 11mmol/L.
2 weeks later I got an email from Boston that I had been accepted. An achievement I believe I only reached because of my type 1 diabetes that gave me the resilience, determination and belief that I could do it.

To finish, here are my top 3 tips for a marathon:
- Trial (and error) everything in training – this is essential so you are prepared for any situation on race day. Not only do you need to trial your pace and refuelling strategy like any other marathoner. As diabetics we need to trial food or gels that will sustain us but won’t spike our BGLs, we need to trial running and testing our BGLs multiple times – having good BGLs is key for good performance.
We also need to trial our approach if we have a low – do we stop and walk for 5 mins or can we continue running and treating at the same time?
How much insulin do we need to give if our BGLs are running high – for me 0.2 units through my insulin pump is more than enough to bring me back in range from a 13mmol/L reading.
- Have a plan for race day – know what you are going to carry on you and how you are going to carry it. I always wear a waist band and take with me a backup insulin pen (in case my pump fails), my BG meter (even though I wear my CGM), hypo supplies and refuelling supplies – a mix of Clif energy bars and apricot slices.
- Make sure you have something to identify you as a type 1 diabetic – where it be a medicalert bracelet or card or a tattoo (only if you like permanent identification like me). This is really important in the case you have a hypo or another marathon related incident like heat exhaustion or dehydration – you want the medical team to know you have type 1 diabetes so they can be aware and treat you correctly.
My final tip – Don’t let diabetes stop you from doing anything you want.
Now let the Boston training begin. See you in April, 2017.